Eulogy at the funeral, 5 August 2019.

Today we not only bury mum, we celebrate her life, reflect on what she meant to each of us, we give thanks, we seek to understand.
With my brother Shane, I thank in particular our magnificent sisters, Maree and Karyn, who cared so deeply, who were mum’s bedrocks, always a great comfort for mum over so many decades.
Mum was a character. She had a twinkle in her eye, a smile splashed with a touch of mischief. Her joy of life was infectious, embracing, and shared.
Over Easter, for 3 weeks, mum stayed with us at Strathfield. Pretty well every grandchild and great grandchild came over. Her visitors at her doorstep, arriving not out of a sense of duty, but because of the jubilation of being with a happy soul.
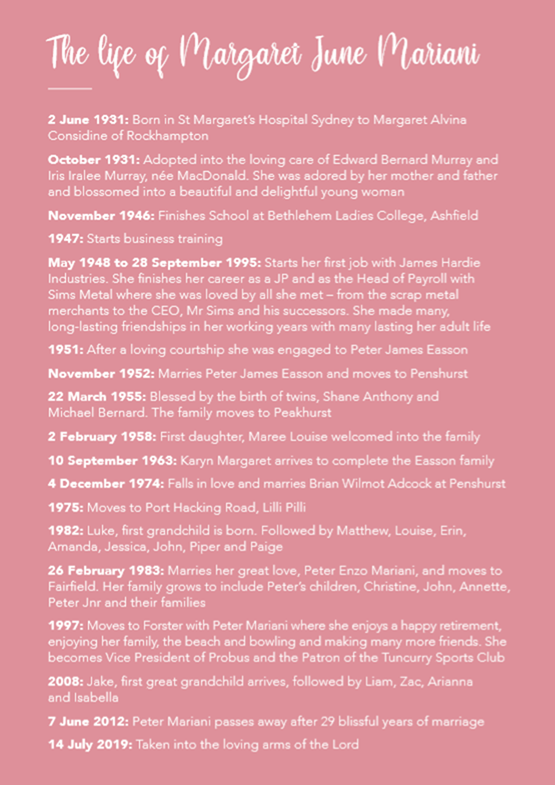
The chronology in the mass-book, and the slide show, conveys a glimpse of the person we knew.
You really know someone through their stories. So let me tell a few.
Mum, as a teenager, on skates – or was it a bicycle? – holding on to the bumper bar of a bus on Parramatta Road, speeding and waving and smiling like there was no tomorrow. Thank God she only did that once.
I think of the holidays we shared, mum’s love of coconut oil and baking in the sun, beach towels, surf, and those hot chips melting into the buttered bread as we squeezed, in Laurieton, North Haven and Byron Bay.
Mum and Masterchef may not be obvious matches, as Shane alluded to, but she instilled in us an appreciation for what good cooking could be!
One night coming home from work last April mum exclaimed – “what is this amazing dish Mary cooked? You cannot believe how good it is. What is it again?”
“Mum, it’s spaghetti bolognese.”
Mum was remarkable and kind – except for that time my sister Maree and I ran away from home, to escape brother Shane. Also when Karyn’s fishbowl – and the fish – was affected by the charitable effort of one of her siblings to turn the water a more attractive shade of blue.
We all knew mum loved us unconditionally and deeply. She hoped we would be better versions of ourselves; wanted us to strive for self-improvement.
One day she took Shane and I to learn boxing. I think I was alright. But there was this sentimental attitude about never separating the twins. So, instead, an hour into our first training exercise, the bossy authorities of the St George Police Boys Club, Hurstville, put us down for the choir. Mum claimed the credit, of course, when we later appeared on the Don Lane television show. Twice.
Another instance of mum’s incredible personality was in Noumea. She was on a cruise. The railings from boat to shore were wobbly and down she went – spending 10 days in hospital in New Caledonia. Maree, Mary, Antonella, & I trecked over. There was one guy in the hospital whose son kept visiting, refilling his big coca-cola bottle every time. I mentioned to mum that it is incredible that someone in hospital would be allowed to drink so much coke.
She beckoned me to lean down and in that conspiratorial whisper explained: “It’s not coke. It’s rum and coke.” Typical of mum to encourage us to buy the poor guy a bottle of whiskey for the next bottle re-fill.
When mum was staying recently at Strathfield, I would get up earlier than the others, and there on the dining table was mum’s breakfast – a bowl of coco pops.
Frankly, I do not care what they say. When you are 88, if you want coco pops in the morning, you are entitled to coco pops in the morning.
Mum believed in God and identified as Catholic. I thank my sister Karyn for organising Father George to administer the Last Rites on that dreadful last night in Taree.
And thank you too, Fr. James, for the magnificence of your service today.
We are all specks of the divine. I truly believe mum had a few more specks than most, naturally cared for more people than is usual, exuded a warmth for others that we can only hope to emulate.
I can also hear her beckoning: “For heaven’s sake, Michael. Don’t make me out to be a saint. They’ll never take me seriously again at the Tuncurry-Forster bowls!”
She absolutely was proud of her brood – her family, children, grand-children, great grand-children, her step-children and theirs too.
So many stories. West Tigers. I am sure there is theological authority somewhere. Her idea of Heaven was of a winning try scored by West against Manly in the dying moments of a Grand Final. Mum’s love of Cadbury fruit & nut chocolates, her thinking about Labor, her love of bowls. That first visit to London, the Langham, the Sound of Music — too many tales to tell. Mum lives on in our memories. We can be inspired by her demeanour, her personality, her love.
We are returning home today. Family can be stronger than blood. As she promised her own mum, our mum will be buried with her adopted parents, who loved her so much.
Mum believed that:
“One short sleep past, we wake eternally
And death shall be no more.”
We know mum is in the embrace of a loving God.
We love you mum. Thank you.




Postscript (August 2025)
Mum was known after 1983 as Margaret June “Betty” Mariani. Her four children, Shane Easson, Michael Easson, Maree Simmonds (née Easson) and Karyn Hemming (née Easson) were to her first husband, Peter James Easson.
A Coronial Inquiry was held into the death of Mum, Mrs Margaret June Mariani who died on 14 July 2019 following complications from cholecystectomy surgery
There was a protracted period of years involving an autopsy, commissioning of expert specialist advice by the family, and representations requesting a Coronial Inquest. The Court, Mum’s family submitted, needed to consider the complications of cholecystectomy surgery, death as a result of peritonitis as a result of a mistake during the operation, grossly inadequate care and treatment provided at Forster Private Hospital – including inadequate monitoring and poor record keeping of observations, and the various delays in notifying the surgeon of deterioration, together with systemic deficiencies in practices and procedures.
Long story short, following seven days of hearings, cross examinations and presentation of evidence, in February 2025, the findings of Deputy State Coroner Joan Baptie were released on 14 August 2025, six years and one month after Mum died: https://coroners.nsw.gov.au/documents/findings/2025/Inquest_into_the_death_of_Margaret_Mariani.pdf
My siblings, Shane Easson, Maree Simmonds, Kary Hemming, and I were determined to understand what happened and what lessons could be drawn to diminish the likelihood of anything similar happening again.
The coroner reviewed the evidence of complications that followed a deficient operation and post-operative care and determined:
335.The resulting care and treatment Mrs Mariani received was significantly deficient in numerous ways.
336 The evidence is capable of establishing that if Mrs Mariani’s symptoms, including her pain and discomfort, had been investigated at the request of her daughter on the morning of 13 July 2019, it is more likely than not that she could have been re-admitted to theatre for a corrective procedure.
337 Mrs Mariani’s death was preventable.
338 The lack of professional review of the systemic issues by Forster Private Hospital are significantly concerning in terms of the health and safety of potential or future patients.
339 Mrs Mariani’s family gave a compelling and eloquent family statement. Their distress and advocacy have been boundless.
The evidence, the magistrate’s findings and recommendations, have now been referred to the NSW Minister for Health and the NSW Health Department for consideration of steps and practices that need to be adopted from here.
The ABC reported the story: https://www.abc.net.au/news/2025-08-14/margaret-mariani-coronial-inquest-findings-private-nsw-hospital/105654490?utm_source=abc_news_web&utm_medium=content_shared&utm_campaign=abc_news_web
My siblings’ and my advocacy for Mum and her community are not over.
One of the solicitors working for the Crown Solicitor was incredibly diligent. After proceedings were over, we heard for the first time that one of the solicitors was jogging in the Botanical Gardens in January 2024 and sat at a bench there where a plaque tributes Mum. I suspect that was an omen which made that solicitor redouble or triple the effort put into doing research.
Submission from Family Members on 26 May 2025
After evidence was heard in February 2025 at the Coroner’s Court, Lidcombe, family members made this submission in response to Counsel Assisting’s representations to the Coroner:
The Deceased Family’s Submission: 26 May 2025.
Introduction and Overview
- With respect to the Coronial Inquiry, Mrs. Mariana’s family are grateful for the thorough evaluation of the evidence that led to her death.
- The family have always said that our main interest, besides finding out how and why death occurred, is to ensure that nothing similar – an act or acts of neglect or poor medical management – happens to any other patient as occurred with our mother.
- We know all medical procedures have an element of risk.
- Reasonably minimising those risks, learning from mistakes and best practice, are therefore paramount in hospital care.
- We believe the coroner must assess whether the evidence of systemic failure in the care of Mrs. Mariani can be written off as likely due to negligence, perhaps centred on one negligent nurse, in particular. Or whether the systemic failures merit critical and thoughtful consideration.
- Of course, systemic failure and negligence are not mutually exclusive. They do not always go together, but they are often joined.
Systemic Failure
- The evidence is very strong about systemic failure.
- In 2020, Professor Duflou summarised his opinion as to the provision of care by Forster Private Hospital thus:
‘There are in my opinion strong indications of systemic and other failures in the treatment of the patient at Forster Private Hospital…
“Such failures not only potentially contributed to the death of the patient, but if such failures are systemic it can be reasonably anticipated that these will be repeated in the care of other patients at the hospital unless corrective action is taken.
“The Forster Private Hospital medical records are in my opinion incomplete, patient interactions are inconsistently documented and there appear to have been examinations of the patient which have not been documented at all. Such poor documentation is a matter of significant concern, not only in relation to the investigation and treatment of this patient, but in relation to patient care in general at the hospital.
“Despite the significant deficiencies in the medical record, there are strong indications that the patient was deteriorating clinically between the time of her surgery and the time of her transfer to Manning Base Hospital…
“The patient was not investigated further until she had collapsed, by which time there had been prolonged deterioration… As such, there appears to have been a serious failure in provision of quality health care in this case…”[1]
- The family believes that against this devastating appraisal, action needs to be taken for the safety of future patients.
Observations on the Evidence
- One of the nurses “caring” for our mother in the post-operative stage at Forster Hospital did not keep adequate records, did not inform other nursing staff of Mrs Mariani’s daughter’s concerns (Ms Karyn Hemming), and did not inform Dr Francis, the visiting medical officer at the hospital, of the parlous state of our Mother’s health, as she tried to recover post the operation.
- Professor Williams thought at relevant times that Dr Francis should have consulted Dr Ghaly.
- Further, Dr Ghaly, who worked long hours at the Forster and Manning Base hospitals on a wide variety of surgical operations can say, even though he intended personally to check the health and recovery of Mum the day after an operation, on Saturday13 July 2019 (and we take him at his word), that no one had told him he had anything to be worried about.
- Interestingly, though, Dr Ghaly says he should have been consulted about Mrs Mariani’s persistent pain and believed Dr Francis should have been in touch with him.[2]
- The family submits that if Dr Duflou’s summation is fair, then Mrs Mariani’s death was avoidable. So, the question before the coroner, we humbly suggest, is whether those failures discovered because of this coronial inquiry require findings that are sufficient to mitigate against reasonably foreseeable mistakes.
- Mum was deemed fit and able for her operation. She believed she would be in good care and was assured the operation would be straight-forward with expected discharge within a day or two.
- We are not medically or legally trained, so we rely on the goodwill, competence, and thoroughness of all involved in these proceedings. Needless to say, we are grateful for these proceedings and respect all involved.
- Further, we are nothing other than sympathetic to the overall sincerity and care of those in our hospital system.
- But we wonder whether the workload and procedures at Forster facilitated the catastrophic disaster that happened.
- The evidence of Ms Karyn Hemming is that she pleaded with nursing staff to send a doctor as her mother was in intense pain.
- Further, Ms Hemming noted her mother was scolded for pressing the PCA button too many times. It was obvious that Mum pushing her knees up to her chest, writhing in pain, and commenting to her daughter on her agony, were red flags.
- After all, pain was not the only signal. There was her vomiting, her physical manifestations, including as Ms Hemming reported to hospital staff, her alarming fatigue and weakness.
- Mum was from a generation that revered authority and didn’t answer back. A stiff-upper-lip was characteristic of her generation.
- We know that overnight, extra pain prescription was prescribed by Dr Francis, who from his witness statements and at the witness examination seems to have little recollection of anything that happened prior to our mother being rushed to Manning Base Hospital.
- Dr Francis, the evidence suggests, was then a medical officer inexperienced in surgery, and should have sought advice from an experienced surgeon. This was certainly so the morning after the operation, when Ms Hemming’s compelling evidence is that her mother required intense evaluation of her medical condition.
- It now clear that Mrs Mariani died due to an accidental cut of the colon which occurred during her operation. This is consistent with the report of Dr Jonathon Murtagh at Manning Base hospital at the time of death, who recorded the cause of death as “aspiration pneumonia secondary to possible intra-gastrointestinal surgical complication from laparoscopic cholecystectomy.”[3]
- This is also consistent with the Autopsy Report of Dr Brouwer which concluded that the direct cause of death was “complications of cholecystectomy surgery.”[4]
- Infection occurred and the associated complications throughout Mrs Mariani’s stay in hospital led to her death. Hospitals are known to be significantly short-staffed on weekends compared to during the ‘normal’ working week.
- We wonder if patients approaching the end of their ninth decade should be operated on and repatriated to the recovery ward on a Friday night, without a mandatory review by the surgeon or a senior medical officer the next day.
- The nurse who attended to our mother complained to Ms Hemming that she was “run off her feet.” How must this be addressed in future? We want great procedures, checklists to follow, and trained staff capable of implementing.
- We wonder if a factor in Dr Francis’ attentiveness to our mother’s pain and Ms Hemming’s pleas was due to his being overwhelmed by his duties in the 24-hours he was stationed at the hospital, from our mother’s discharge to the recovery ward to when she was transported to Manning Base Hospital.
- Additionally, questions arose in the witness examination as to what guidelines were given or expectations conveyed to Dr Francis as to what to do and look for with this patient. The absence of adequate hospital checklists is of grave concern to the family.
- At the Coronial Inquest, evidence was given of Dr Ghaly working long hours at both Forster and Manning Base Hospitals. It is a reasonable inference that he was exhausted on some days, and probably his absence from seeing our mother at Forster Hospital can be explained, at least partially, the day after her Friday operation, because he wanted to rest before returning to his rounds.
- We say a reasonable person would conclude that the staffing arrangements, training and checklists associated with how Forster Hospital is managed is in critical consideration.
- In the evidence there are references given to the London Protocol and their review and amendment at the Hospital, following Mrs Mariani’s death.[5] We have not sighted such.
- The deep question is whether this is sufficient to mitigate the risks associated with this happening again. We trust the Coroner in her assessment here.
- What is clear is that there was systemic failure. No one picked up or amplified concerns to senior medical staff that our mother was well “outside of the flags” of expectations and seriously ill, in unrelenting pain, and that steps needed to be taken for proper, rigorous investigation and action.
- Complacently was the enemy of good medical care. Our mother did not receive the care she deserved.
- Dr Markowskei eloquently spoke, if defensively, for his clients. Yet, surely, Professor Williams’ evidence, based on his extensive surgical experience is to be preferred, where there is conflict on the evidence.
- Because records, relating to our Mum’s treatment, were so haphazardly collected, it is difficult to fully appraise the ‘trip points’ leading to death.
- It is concerning that RN Martyn claimed she was not educated about filling in the various forms.[6]
- Nonetheless, whether RN Martyn’s excuses are believed, Professor Williams opined that the degree of sudden decline in the patient was not consistent with the record of hospital notes. He was adamant that Mrs Mariani’s case was well outside the expected course. And that Mrs Mariani was deteriorating throughout the day.
- Significantly, Professor Williams considered that the record keeping per se was not so much of a concern, compared to the lack of action in response to pleas from Ms Hemming, associated with lack of awareness of a deteriorating patient and the absence of Dr Ghaly.[7]
Conclusion
- The family appreciates the diligence of the Coroner, Counsel Assisting, the Crown Solicitors Office, and all who have participated in this inquest to discover truth and learn appropriate lessons.
- We know how difficult this can be in sifting through contested evidence, where conclusions on some points can only be approached hesitatingly. Yet we see that there were systemic failures.
- Neither of us are medical or legal experts; we can only pray that all Coronial findings and recommendations are made in single-minded focus as to whether this inquest has done its job in mitigation of comparable or similar mistakes happening again.
Submitted by the following of Mrs Mariani’s children:
Dr Michael Easson AM [not a medical doctor]
Mrs Maree Simmonds
Ms Karyn Hemming
[1] Tab 39, Expert Report of Professor Johan Duflou, 19 October 2020, pp. 7-8.
[2] T. 5/2/25, p. 39, lines 42-47.
[3] Tab 4-Verification of Death, 14 July 2019; Tab 45, Manning Base Hospital Progress Notes, 14 July 2019, p. 22.
[4] Ref. Foster Private Hospital Records, Tab 5, pp. 18-22. Tab 2, Autopsy Report for the Coroner, 11 May 2020, pp. 2,5.
[5] Volume 2 of the Brief of Evidence.
[6] T.10/2/25, p. 179, lines 9-10.
[7] Tab 41, Export Report of A/P Nicolas Williams dated 20/05/24, p. 2.
Note: We cannot speak for our brother, Shane Easson, who is presently overseas.
26 May 2025
Representations Made to the Coroner in November 2020
Mum’s children were keen that an inquiry be held into the cause of death and what should be learnt from mum’s death. On behalf of Mum’s children, I made this representation to the NSW State Coroner:
NSW State Coroner,
Office of the State Coroner,
1A Main Avenue,
Lidcombe NSW 2141.
18 November 2020
Your Honour,
I refer to the decision by Coroner Magistrate Shields as advised on 10 November 2020 by Mr A.J. King, Registrar, Local Courts, Taree and Forster, to Mr Michael Hempsall, of Uther Webster & Evans (UWE) solicitors, concerning matter number 2019/00219251, relating to the death of my Mother, Mrs. Margaret June “Betty” Mariani (02.06.1931-14.07.2019) who died in the early hours of the morning in Manning District Base Hospital from complications of cholecystectomy surgery performed in the latter part of the afternoon on Friday 12 July 2019.
Mr King advised: “Following consideration of relevant advice from police officers and medical practitioners, and other appropriate persons, the Coroner is satisfied that the date, place, manner and cause of death of Margaret Mariani have been sufficiently disclosed. Consequently, pursuant to section 25 of the Coroner’s Act 2009 the Coroner has dispensed with the holding of an inquest.”
Notwithstanding this view, I respectfully request that under S.29 of the Act, for the reasons outlined here, and other supporting documentation put forward by the family, including the family’s legal advisers (UWE), that an inquest be ordered to investigate the systemic failures which led to an unnecessary death.
There are valuable lessons that can be garnered to improve attention to foreseeable complications and thereby prevent loss of life. Checklists need to be adhered to such that warning signs are detected early to prevent fatal consequences.
Mum would want her family to do nothing less than to protect the community she loved and to heed the lessons from this unfortunate episode.
I make this submission with the support of my three siblings and as Mum’s son.
Systematic Failures Require an Inquest
I know that coronial inquests are usually only conducted where there are concerns relating to widespread and systemic issues. It appears that Coroner Magistrate Shields believes that the family’s concerns fall short of establishing systemic failure.
I respectfully suggest that this conclusion is not warranted on the evidence and that, on the contrary, an inquest is merited.
In this context, I note that on your appointment on 15 July 2019, coincidentally a day after Mum’s death, it was noted: “Magistrate O’Sullivan has a strong interest in the death prevention function of the coronial jurisdiction and the Court’s role in achieving systemic, social and economic benefits for the community as a result of its work. See: https://www.justice.nsw.gov.au/Pages/media-news/news/2019/Announcing-NSW’s-new-State-Coroner.aspx
Those words call attention to core principles. Whether in a particular death any failures were significant and systemic, and if there are social and economic benefits that merit the time and resources required for an inquest.
I believe that if a death is due to systemic failure and the chain of causation can be reasonably established, then genuine social and economic benefits are realisable through informed practices that apply lessons that can be learnt.
If this reasoning is accepted, then the issue to be determined is whether Mum’s death was preventable, due to more than individual failings, and was indeed a consequence of systemic failure.
The evidence prima facie shows this is the case and therefore the inquest should occur.
The Facts
- For cholecystectomy surgery, Mrs. Margaret June “Betty” Mariani, a woman of 88 years was operated on in the afternoon of Friday 12 July at Forster Private Hospital with Dr Moheb Ghaly as the operating surgeon.
- Earlier, in May 2019, Mrs Mariani had been treated for severe pancreatitis, including a brief period of hospitalisation;
- Mrs Mariani’s daughter, Mrs Karyn Hemming, accompanied Mrs Mariani to the Forster Private hospital on Friday 12 July, and was with her on release from surgery that night, and early the next day, Saturday 13 July, and to the early hours of Sunday, 14 July 2019.
- Mrs Hemming consistently reported to doctors and nurses from post-operative “recovery” to Mrs Mariani’s transfer to Manning District Base Hospital on the afternoon of 13 July 2019, that her mother was persistently in severe pain and vomiting.
- Mrs Mariani died at around 3.00am on 14 July 2019 at Manning District Base Hospital.
- A postmortem report dated 24 July 2019 was prepared by Dr Issabella G. Brouwer and identifies the cause of death to be “complications of cholecystectomy surgery.”
- Observations are made in Dr Brouwer’s report as to the circumstances and a significant pathological finding is this: There was a
SMALL BOWEL PERFORATION WITH ASSOCIATE PERITONITIS – perforation of the small bowel at site of adhesion of bowel to the anterior abdominal wall in vicinity of para-umbilical surgical incision. Surgical suture material at site of adhesion. Sections of the adhesion and para-umbilical surgical incision showed extensive acute inflammatory cell infiltrates, pus collection and associated necrosis of tissue.
It is reasonable to conclude that this accidental incision of bowel tissue led to Mrs Mariani’s death.
Police Constables’ Statement.
A statement dated 6 August 2020 by Senior Constables Larrain and Pritchard, inter alia states:
- Of note, I have had significant difficulty in obtaining statements from any medical staff represented by the Nurses and Midwives Association. All of which has been recorded by email and forwarded to the Assistant to the Coroner.
- I am not a medical professional but based on my limited knowledge of the field and reviewing statements and medical records I have compiled, I am of the opinion that the deceased was aware that death was a possible outcome of the elected surgery. I also believe that her documented poor health, her advanced age and the trauma associated with prolonged anaesthesia and surgery (regardless of it being routine in nature) to be the main course of her death.
Comment 17 is interesting about the difficulty of obtaining statements from the medical staff. Comment 18 looks somewhat unusual. I am not even sure why and on what basis this was made. No one from the family was interviewed.
Dr Duflou’s Observations
As the family had not seen the full Autopsy report until a few months ago, we engaged Dr Duflou, a specialist forensic pathologist at the Forensic Medicine Centre, Canberra, to review the evidence and make observations on the evidence to hand. He summarises the matter:
There are in my opinion strong indications of systemic and other failures in the treatment of the patient at Forster Private Hospital if the discrepancies as identified in this commentary are in fact correct. Such failures not only potentially contributed to the death of this patient, but if such failures are systemic it can be reasonably anticipated that these will be repeated in the care of other patients at the hospital unless corrective action is taken.
The Forster Private Hospital medical records are in my opinion incomplete, patient interactions are inconsistently documented and there appear to have been examinations of the patient which have not been documented at all. Such poor documentation is a matter of significant concern, not only in relation to the investigation and treatment of this patient, but in relation to patient care in general at the hospital.
In essence, those observations are compelling as to the merit of an inquest.
Reasonable Presumptions
On the evidence, particularly the autopsy report, it is clear there was a perforation of the bowel (small intestine) at the time of the cholecystectomy. This is certainly a recognised complication that can occur to any surgeon, particularly in a patient who has had pancreatitis in the recent past, as there would be increased scarring and inflammation around the gallbladder, and this makes the surgery more difficult.
Causing a perforation at the time of surgery is not an unheard of complication and ordinarily would be regarded as an unfortunate event. I have consulted with specialists and am advised that in such circumstances ideally the surgeon immediately realises the unfortunate event has happened and then the surgeon opens the abdomen to wash out any spillage, repairs the perforation, and completes the operation as a traditional open cholecystectomy (rather than ‘keyhole’).
If the unintended perforation is not identified immediately, the patient develops peritonitis. This, initially, might be somewhat limited, and might even stabilise for some time, but then it becomes generalised and the patient deteriorates rapidly. If it is identified early, the patient needs reoperation to clean up inside and repair the damage, more or less as above. If this occurs promptly, things should be okay, but nothing is guaranteed.
The real issue in this case is the delayed recognition and hence lack of response till it was too late.
Given the degree of peritonitis present, it is certain that the perforation happened at the time of surgery.
The unusual amount of pain experienced by Mrs Mariani is a sign of this potential problem, though recognising that pain is difficult to assess.
A careful assessment on the night of Friday 12 July 2019 after Mum’s operation or early the next morning may have raised suspicion of problems.
But as we know from Dr Ghaly told the family (on the Tuesday after Mum’s death – I was on the call) he had not been told there were any complications and he had found it difficult to get through to the hospital (phones ringing out; messages not taken) on the Saturday morning.
We cannot be certain, but if there was alertness to the potential issue, if Mum had had corrective surgery then her chances of full recovery would have been possible. Unfortunately, Mum then developed generalised peritonitis. Even in someone in good health this is a bad outcome and left to fester it can be unsurvivable. In summary, the major issue of concern is not that Mum had a bowel perforation, but that it was not identified and dealt with (by reoperation) either at the time or when the signs became apparent post-operatively. The delay of some 18 hours or more before there was any serious response was catastrophic.
Forster Private Hospital Management
Working back from the finding that Mum died from complications of cholecystectomy surgery, the family assumed that there would be further assessment & reporting by the Coroner’s office.
The family’s understanding is that Forster Private evaluated its procedures as per the London Protocol, relating to a systems analysis.
Although useful, this is surely but one limb of the investigations that are necessary. Indeed, as the US institute for Healthcare Improvements summarises:
The purpose of the London Protocol is to ensure a comprehensive and thoughtful investigation and analysis of a clinical incident, going beyond the more usual identification of fault and blame. A structured process of reflection is generally more successful than either casual brainstorming or the suspiciously quick assessments of “experts.”
The approach described in this protocol does not supplant clinical expertise or deny the importance of the reflections of individual clinicians on an incident. Rather the aim of this approach is to utilize clinical experience and expertise to the fullest extent, and to assist the reflective investigation process. (http://www.ihi.org/resources/Pages/Tools/SystemsAnalysisofClinicalIncidentsTheLondonProtocol.aspx)
The family believes that given the limitations on the evidence gathered to date, referred to in the police constables’ statement, etc., that through an Inquest, inquiries and evaluations should prove insightful to ensure that the risk of a death in the future can be minimised, such that steps are taken that learn from our Mother’s experience, to the benefit of others.
Some questions were raised by the family in email correspondence to the hospital in August and forwarded to the Court Registrar. These might be explored by an inquest, including:
- Whether an operation for any person over 85 at a country hospital should occur on a Friday afternoon?
This, especially because of the lack of staff resources typically rostered on a weekend.
- Why the time date of the picture scan of mum’s gall bladder, supposedly taken after the operation, was inaccurate?
I now understand in consequence of the family’s representations, and in accordance with the London Protocol review, Forster Private have now recalibrated the timing mechanism of its equipment in the operating theatre.
- Whether the x-ray scan of mum’s lungs taken on Saturday afternoon at 4.11pm (on our copy) was also time dated correctly?
We asked that this be checked.
- Whether the x-ray of Mum’s lungs apparently taken on the late Saturday afternoon indicated fluid on the lungs and, perhaps, evidence of aspiration?
- Whether more urgent and considered attention could have been given when mum was at Forster Private, especially given the potential for infection?
- Whether Dr Ghaly should have been better informed of what was happening to Mum post the operation?
I and my siblings were told by him on Tuesday 16 July in a telephone call that he had been unaware of Mum’s deteriorating condition. That he had tried to call three times the hospital on the Saturday (13 July) and finally got through and was told everything was ok.
- Whether Dr Ghaly should have seen Mum after the operation at Forster Private?
I ask if this was unusual for this not to have occurred. If he had of heard of Mrs Hemming’s concerns and noticed the symptoms, if Mum’s life could have been saved?
After Mum was rushed by emergency ambulance from Forster Private to Manning District Base Hospital late on the Saturday afternoon (13 July) Dr Ghaly rushed to Manning and immediately suggested that he operate – suggesting he instantly recognised the likely complication. But it was too late. (Mrs Hemming witnessed this.)
- Whether mum received sufficient care during the evening when she was continuing to be in considerable pain?
Forster Private Hospital administration told the family that their notes of Mum’s hospital stay included a chart which indicated that pain management had improved and some sort of happy equilibrium was the status before Mum took a turn for the worst. But as the preliminary autopsy points to Mum’s death as having been caused by severe peritonitis as a result of complications from her gallstone operation, it is inconceivable that this illness suddenly erupted. All the evidence points to rapid deterioration over a 24-hour period.
- Whether blood tests were taken before the operation that indicated any reasons for concern?
Is this usual practice? If not, why not?
- Whether the hospital is sufficiently on alert for peritonitis and like infections?
The family is left wondering whether the peritonitis risk was inadequately assessed.
- Why no doctor saw Mum but for a visit by Dr Williams on the Saturday morning, July 13?
The doctor was in a rush, and only visited at Mrs Hemming’s insistence; he appeared unalarmed by any warning signs, and merely recommended extra pain relief.
- Whether the clear evidence of severe pain (nurses ringing in the middle of the night pleading for a doctor’s assistance) is consistent with the equilibrium chart, also referred to above?
The concern of the nurse in the evening is recorded in the Forster Private Hospital notes (which we doubt were reviewed by the local Coroner’s office). It seems clear there was insufficient cognisance of the signs of Mum’s enveloping peritonitis.
- Whether the shifts of surgeons and supporting staff is conducive to good medical practice. Is it true that the custom is with busy surgeons is to work 12-hour to longer shifts? If so, the question arises: is this safe?
The family are interested to know Dr Ghaly’s surgery hours that week. Was he too exhausted to check on Mum? This is not to attack him, especially given limited experienced medical staff in the regions, but it is relevant in this instance.
The answers to the questions we ask, we believe, are in the interest of the community that mum loved and spent the last decades of her life.
Conclusion
The family is not seeking revenge or wants to pursue insurance claims. We want to address systemic failures that arose from failing to look out for potential, foreseeable complications. Checklists to watch out for what Mum might have endured were not followed. It is interesting in the light of these representations to reflect on observations by Dr Atul Gawande, the American surgeon, writer, and public health researcher, whose influential book The Checklist Manifesto: How to Get Things Right, Henry Holt and Company, New York, 2009, addresses better health care management by health professionals. Gawande notes the importance of checklists: “…under conditions of complexity, not only are checklists a help, they are required for success.” “One essential characteristic of modern life is that we all depend on systems—on assemblages of people or technologies or both—and among our most profound difficulties is making them work.” “Good checklists, on the other hand are precise. They are efficient, to the point, and easy to use even in the most difficult situations. They do not try to spell out everything–a checklist cannot fly a plane. Instead, they provide reminders of only the most critical and important steps–the ones that even the highly skilled professional using them could miss. Good checklists are, above all, practical.”
If from our learnings, through revitalised procedures & systems, we ensure a greater safety, the family knows we thereby honour Mum’s support for her community.
We trust that these representations are carefully considered.
Yours sincerely,
Dr Michael Easson AM FRICS FAICD







